- Home
- |
- About
- |
- Patient Information
- |
- Laser
- |
- Surgery
- |
- Referral Process
- |
- FAQs
- About Basic Eye Anatomy
- About Glaucoma
- About Common Glaucoma Medications
- About Common Eye Antibiotics
- About Anti-Inflammatory Eye Drops
- About Eye Supplements
- About Posterior Vitreous Detachment, Retinal Tears and Detachment
- About Macular Degeneration
- About Diabetic Retinopathy
- About Dry Eyes, Blepharitis and Ocular Rosacea
- About Corneal Abrasions
- About Contact Lens Infections
- About Conjunctivitis
- About Iritis
- How do I apply eye drops?
- How do I apply eye ointment?
- About Preventative Eye Care
- |
- Links
- |
- Contact
XEN® Implant
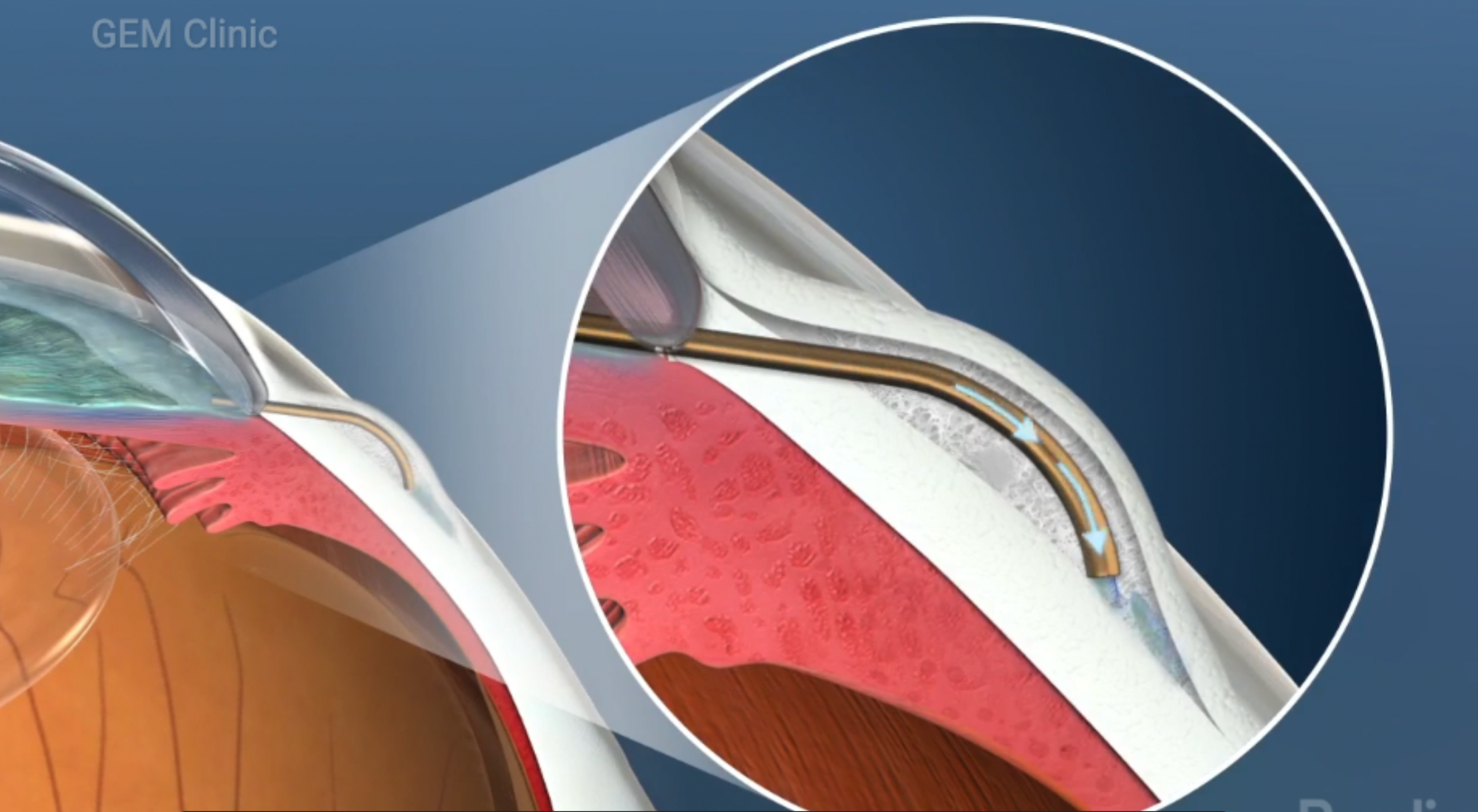
Picture shows placement of a XEN® implant inside the front of the eye, creating a new drainage pathway for fluid to exit the eye and leading to lower eye pressure. Image is blown up to show XEN® implant inside the inner layers of the eye. (picture courtesy of Rendia)
About XEN®
What is a XEN® Gel Stent?
A XEN® Gel Stent is a surgical implant measuring 6mm in length and made of porcine collagen. It is used to treat open angle glaucoma. It is implanted inside the front of the eye to bypass the natural drainage canal and provide an alternate drainage pathway for aqueous fluid to leave the eye. Improved drainage from the eye allows the eye pressure to decrease into a more acceptable and safe normal range. This prevents worsening of glaucoma damage to the eye and loss of vision.
Are there different types of XEN® implants?
The XEN® Gel Stent comes in two different lumen (internal diameter of the stent) sizes, XEN®45 (45 micron lumen size) and XEN®63 (63 micron lumen size). The larger the lumen, the more fluid can pass through. Your surgeon will review the pros and cons of using one size over the other and which option would be safest and most effective for you.
Does a XEN® Implant show up on an X-Ray, CT scan or MRI? Is it MRI-safe?
The XEN® Gel Stent is made out of porcine collagen, therefore it is not radio-opaque and does not have any metal in it. It will not be seen on an X-ray or CT scan. Theoretically, if the MRI images are very focused, it may be visible on an MRI. It can be seen on an ocular ultrasound or OCT of the anterior chamber of the eye.
It is safe to have an MRI with a XEN® implant since it is not made out of metal.
How is XEN® surgery performed?
A XEN® Gel Stent can be implanted into the eye from the inside of the eye (ab interno), or from the outside (ab externo). Generally, implantation from the inside is faster, but can also be technically challenging and therefore, most surgeons prefer to implant from the outside of the eye. This allows for dissection of the surface tissues of the eye to avoid plugging of the stent as in is implanted. Mitomycin C is an anti-metabolite drug used during this surgery to reduce scarring and surgical failure (see below for details). After surgery, 5-fluorouracil, another anti-metabolite, may also be used an an eye injection to reduce scarring. These treatments may be performed at follow-up clinic visits.
What are some of the risks of XEN® Implant surgery?
In general, XEN® implant surgery has similar potential complications when compared to traditional trabeculectomy surgery for glaucoma. However, the complications are less frequent, recovery is faster, vision is less blurry for less time, and there are overall less frequent post-operative visits.
Vision is blurry after the surgery but there is a faster recovery compared with trabeculectomy surgery. Rarely, especially if you already have very severe glaucoma damage to the optic nerve, you can suffer further permanent vision loss after surgery. This is rare, but can happen, even with routine, uncomplicated surgery. Other possible complications can include very high or very low pressures after surgery, over drainage of fluid causing collapse of the front chamber of the eye (rare with XEN®45; can occur with XEN®63 but can be prevented with the use of a partial suture plug), wound leak, accelerated development of cataract, bleeding during or after surgery (which can be minor or major causing usually temporary but sometimes permanent vision loss), infection (rare but when severe can cause loss of the eye) or retinal detachment (rare with XEN® surgery alone, but higher when cataract surgery or vitrectomy is done at the same time). Rarely, the XEN® implant can become exposed and require removal to prevent infection. (Please note: This is not an exhaustive list, but covers the most note-worthy potential risks.)
Please note that although this is a scary list of possible complications, most of these issues are treatable with reasonable ultimate outcomes. If you encounter a complication, every effort will be made to remedy the situation as much as possible, including further medication, laser or further surgery as needed. Your surgeon will discuss these options with you. Your patience and cooperation is greatly appreciated during this time since this will help the healing process immensely.
What is Mitomycin C (MMC) and why is it used for XEN® surgery?
Mitomycin C (MMC), a drug used in chemotherapy, has been a useful tool in glaucoma surgery to prevent scarring of the tissues around the stent, causing it to be plugged. MMC is used either as a minute injection prior to dissection of the conjunctiva (outer tissue later of the eye), or applied with MMC soaked sponges under the conjunctival and Tenons (fascial layer) after it is opened up. If sponges are placed, they are removed after a certain number of minutes, and the area is thoroughly rinsed. Care is taken to avoid exposing the edges of the wound and the inside of the eye to MMC. Without the use of MMC, the XEN® implant would eventually become blocked due to scarring, filtration would stop and the surgery would be unsuccessful.
What are the risks of using Mitomycin C and 5-Fluorouracil drugs in the eye?
These medications are anti-metabolites that prevent new cell growth. They are used to stop fibroblasts or scar-making cells from growing. They can sometimes affect the growth of normal cells, and cause delayed healing, persistent wound leak or thinning of the surrounding tissues, or corneal roughness and irritation. These drugs are used on the surface of the eye and are applied cautiously to prevent problems with the wound. However, if they get inside the eye, which is extremely rare due to the way they are used, they can potentially cause damage to the cornea, lens and other structures in the eye. A non-healing wound leak will be repaired by your surgeon since it can lead to infection, bleeding or very low pressures that all can cause poor vision or vision loss. Symptoms of such problems would be eye pain, excessive tearing, redness, or vision loss. If you experience these symptoms, you should contact your surgeon's office, or after hours, go to Misericordia Health Centre or your local emergency department as soon as possible.
Why am I being offered surgery if there are so many risks involved?
The reason you are being offered surgery, is because you are already at risk of losing more vision if your eye pressure remains uncontrolled. You are being offered surgery at this point because the benefits of doing surgery now, outweigh the possible risks.
After XEN® surgery, will the pressure stay in the normal range and my glaucoma be cured?
Successful XEN® surgery will ensure a low pressure for several years, sometimes requiring extra glaucoma drops to help keep the pressure down. Unfortunately, this effect may last 5 to 10 years (or more or less) and then another procedure or a revision of the surgery will have to be done to maintain an acceptable eye pressure. It is important to understand, that glaucoma is a progressive disease that changes over time. Regular monitoring and check-ups will ensure that you are keeping up with the changes. Although we cannot cure glaucoma, we can treat it effectively to help prevent significant vision loss during your lifetime.
If the pressure is still too high after surgery, does this mean the surgery failed?
In order to work, the XEN® tube has to remain unplugged. Unfortunately, especially in the early part of the recovery period, our body's natural tendency to close wounds will sometimes cause too much scarring around the implant. This can lead to blockage of the implant. During the surgery, your surgeon will use Mitomycin C, an anti-scarring medication used in chemotherapy, in very minute doses to prevent scarring. However, despite this, excessive scarring can still occur. Therefore, in the weeks right after surgery, careful monitoring and extra treatment is done to make sure the XEN® heals without too much scarring. You should expect several visits with your surgeon during this time.
What additional steps might your surgeon need to take to ensure that the XEN® is functioning properly?
These steps may include: putting you temporarily (or in some cases permanently) back on glaucoma drops, or doing a series of 5-FU (Fluorouracil) injections to the superficial surface of the eye. 5-Fluorouracil is another anti-scarring, chemotherapy medication used in minute doses to work against aggressive scarring in the early days or weeks after the surgery. At GEM Clinic, it is done in the office, on a weekly or biweekly basis for up to 5 injections (or as needed). Occasionally, you may need a revision if the XEN® stops working due to being plugged by a thick scar.
After all these efforts, if you still do not have good pressure control, you may need to have another type of surgery called Glaucoma Drainage Implant (Device) surgery with either an Ahmed or Baerveldt Glaucoma Drainage Device.
Why am I having XEN® surgery instead of just proceeding to an Implanted device like an Ahmed or Baerveldt implant?
If you are having glaucoma surgery for the first time, XEN® implant surgery is a good initial step that does not involve as much disssection as with a traditional trabeculectomy. When a XEN® implant works well, it can lower the pressure to almost as low as the trabeculectomy with less potential complications. It is usually a shorter operation than both the trabeculectomy and the Ahmed and Baerveldt surgeries, with less frequent follow-ups. However, if you need to have a second glaucoma surgery, an implanted device may be the appropriate next step.
How long will the surgery take?
Routine XEN® surgery will take about 20-30 minutes (longer if any problems arise). When combined with cataract surgery, it can take up to an hour. You will need to be at the hospital 1.5 hours before your surgical time so that the hospital staff can get you ready for the surgery. After your surgery, you will have about 30 minutes to recover, and then will be able to go home. Usually, the entire visit for day surgery at the hospital will take about 4 hours.
Will I have a lot of pain during or after the surgery?
You will be well frozen with local anaesthetic around the eye, therefore you should not feel anything during surgery. If you do have any discomfort or pain, you will be able to tell your surgeon this, and more anaesthetic will promptly be applied.
It is normal to feel some discomfort and irritation from the superficial stitches, and some light sensitivity after surgery. The vision is usually blurry initially.
Symptoms such as severe pain, headache, vision loss, nausea and vomiting are unusual. If you experience any of these symptoms, you should contact your surgeon's office, or go back to Misericordia Health Centre immediately.
How will my vision be after the surgery?
XEN® implant surgery is much different than routine cataract surgery. Blurred vision after XEN® implant surgery (alone or combined with cataract surgery) can last for several weeks after the surgery with steady improvement. When you have cataract surgery combined with any type of glaucoma surgery, you will need to get your glasses updated about 2 months after the surgery when things are stable. In comparison, when you have cataract surgery alone, you can update your glasses at least 1 month after surgery.
Rarely, especially for people who already have severe damage to their optic nerves from glaucoma, surgery can worsen vision permanently. This is rare, but can happen even with uncomplicated surgery. This may happen because the optic nerve in a person with advanced glaucoma may be too weak to tolerate the surgical trauma. Sometimes, a decision is made to avoid surgery, since the risk of losing vision is too high. However, in most cases, if there is persistently high eye pressure, surgery must proceed regardless of the risks, in order to prevent further damage to an already weakened nerve. Your surgeon will discuss the risks and benefits of surgery with you ahead of time, so that you can make an informed decision for your future eye health.
General Information
Where will the surgery be done?
Currently, all eye surgeries offered by doctors at GEM Clinic are performed at the Misericordia Health Centre.
How do I prepare for eye surgery?
What kind of anaesthesia will I be getting? Will I be asleep during the surgery?
This surgery is done with a local anaesthetic and intravenous (IV) sedation. You will be awake but sleepy during the surgery. This is much safer than using a general anaesthetic. You will not be able to feel anything. If you have any discomfort, more freezing will be promptly applied.
What are the potential risks of local anaesthesia?
Anaesthetic complications are extremely rare but can happen even with the small amount of intravenous medications and local anaesthetics that are used. Most of the time, if a patient is comfortable, no drugs are used. However, if a patient is nervous and needs something to stay relaxed, a small amount of sedatives and painkillers are used in the intravenous. In some patients, use of local anaesthetics in and around the eye can cause decreased vision, bleeding and nerve changes. These effects are usually temporary and resolve with time. Rarely, there can be permanent damage. In rare patients with multiple medical problems, these drugs can potentially cause cardiac or neurological problems, resulting in serious illness or even death. We are certainly vigilant of any concerns with the use of medications in our patients and are prepared to deal with these kinds of emergencies. However, we cannot always predict when a serious drug reaction will occur. Thankfully, these complications are extremely rare with local procedures.
Are stitches used? Are they permanent?
A semi-permanent stitch is used to hold the implant in place. Since XEN®63 has a larger lumen size, it can cause more sudden pressure lowering right after the surgery which can lead to some early complications. To prevent this, the a semi-permanent suture is fished through the implant and buried within reach. This partially blocks the tube so that fluid does not flow out too quickly. It can be pulled out weeks or months later to allow for more fluid flow as the eye heals and the pressures starts to creep up again.
The surface skin is closed with dissolvable stitches (or "sutures") that you may feel a little in the first few days after the surgery. However, they usually soften after a few days and disappear within a few weeks. Occasionally, your surgeon will remove them for you.
Will I need to stop any blood thinners?
Yes, it is advisable to stop aspirin or aspirin-like drugs such as Plavix® (clopidogrel) and Ibuprofen at least one week prior to this surgery. Coumadin® (warfarin) or Xarelto® (rivaroxaban) should be stopped at least 2-3 days prior to the surgery. These should be stopped in consultation with your family doctor or specialist. If there are any concerns about stopping these medications, please inform your surgeon. You can restart these about 3 days after surgery, unless otherwise stated.
Are there any herbal medications that cause blood thinning, and which should be stopped prior to glaucoma surgery?
Yes, St. John's Wort and Gingko biloba should be stopped about 1 week prior to glaucoma surgery, because they can promote bleeding during or after surgery.
When can I restart the blood thinners after surgery?
Unless otherwise advised, you can restart your blood thinners 3 days after surgery.
Will I still need to use drops after the surgery?
There are a few drops you will need to take after surgery to prevent infection and control inflammation. Your glaucoma drops are stopped after the surgery, but may be restarted if the pressure is still too high.
What instructions will I be given after surgery?
You will be given an appointment to see your surgeon the next day and a detailed instruction sheet before leaving the hospital. Your prescription will be faxed to your pharmacy before your surgery. Your eye will be covered with a clear plastic shield after the surgery. You can take the shield off at home and start using the new eye drops. You will need to cover your eye with the shield at night for 2 weeks (or as instructed).
Will I have to stay overnight in the hospital?
If you do not have anyone who can stay at home with you, we will arrange for you to stay overnight in the hospital. It is important to have someone stay with you the night of your surgery, because any sedatives used may make you may feel drowsy after the surgery.
Will Homecare be arranged for me, in case I cannot manage all the drops myself?
Please let us know if you require help with your drops and we can arrange for this prior to your surgery. If you already have homecare, please let us know and we will forward all the necessary updated orders to your homecare nurse prior to the surgery.
When can I start driving after the surgery?
Your surgeon will advise you when you are able to drive again.
What restrictions will I have? How long should I be off work?
You will need to avoid any action that increases the pressure in your head during the first two weeks after surgery. This includes things like heavy lifting (10lbs or more), bending over from a standing position, sexual intercourse and being constipated. Be sure to let your surgeon or doctor know if you need a stool softener for constipation. You should avoid any dusty or dirty environments. You should avoid smoking since this may cause a delay in wound healing. This would be a good opportunity to try and quit smoking. You should eat a balanced and healthy diet and keep well hydrated. Do not get direct water into your eyes for about 3 days after the surgery. You may wipe the eyelids with a warm, wet face cloth gently, without applying pressure to the operated eye.
Wear the plastic shield provided over your eye at night for the first 2 weeks. Avoid any appointments to the dentist the first 2 weeks after surgery (as dirty matter can spray into your eye and cause an infection).
Generally speaking, it is recommended that you observe these restrictions for at least 2 weeks after surgery, and stay off work for at least 4-6 weeks, to ensure that you have adequate time to heal.
When can I travel?
You should plan to stay close to the city for at least 6-8 weeks after glaucoma surgery. You will need regular visits to your surgeon to make sure everything is working and healing well. Do not book vacations without checking with your surgeon first.
Can I go to the dentist after eye surgery?
It is not advisable to visit the dentist right after eye surgery. The human mouth is very dirty, and any spray that gets in the eyes from teeth cleaning or dental procedures could cause a very bad infection. Wait at least a month after eye surgery before going to the dentist.
B221-2025 Corydon Avenue, Winnipeg, Manitoba, Canada, R3P 0N5
x204-992-4000 Aassistant@gemclinic.ca
Contact Us
221-2025 Corydon Avenue
Winnipeg, Manitoba, Canada, R3P 0N5
x 204-992-4000 G 204-992-4006
A assistant@gemclinic.ca
Quick Links
Territory Acknowledgment:
GEM Clinic Medical Corporation is located on Treaty 1 territory, the original lands of Anishinaabeg, Cree, Oji-Cree, Dakota, and Dene peoples, and on the homeland of the Métis Nation. We respect the Treaties that were made on these territories, we acknowledge the harms and mistakes of the past, and we dedicate ourselves to move forward in partnership with Indigenous communities in a spirit of reconciliation and collaboration.
Copyright © 2024 GEM Clinic Medical Corporation. All Rights Reserved.